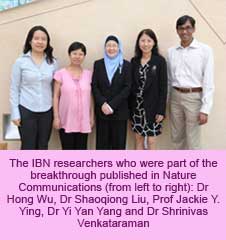
Researchers at Singapore’s Institute of Bioengineering and Nanotechnology (IBN) and California’s IBM Research (IBM) have discovered a new, potentially life-saving application for PET. They have successfully converted PET into a non-toxic biocompatible material with superior fungal killing properties. As reported in Nature Communications, their new material proved particularly effective in destroying drug-resistant fungi and fungal biofilm, displaying great potential as an antifungal agent to prevent and treat topical fungus-induced diseases such as skin infections and keratitis.
IBN Executive Director Professor Jackie Y. Ying shared that, “A key focus of IBN’s nanomedicine research efforts is the development of novel polymers and materials for more effective treatment and prevention of various diseases. Our latest breakthrough with IBM allows us to specifically target and eradicate drug-resistant and drug-sensitive fungi strains and fungal biofilms, without harming surrounding healthy cells. We hope to eventually apply this technology clinically to help the large number of patients worldwide who suffer from fungal infections.”
In recent years, the number of opportunistic fungal infections has increased due to growing populations of patients with weakened immune systems, for example due to cancer, organ transplant or HIV/AIDS. In such patients, invasive infections caused by Candida, Aspergillus and Cryptococcus neoformans (C. neoformans) fungi strains may take the form of potentially lethal blood stream infections, lung infections and meningitis. Candida, for example, causes candidiasis, which is the fourth most common fungal blood stream infection among hospitalized patients in the US, according to the Centers for Disease Control & Prevention.
BCC Research reported that the treatment cost for fungal infections was US$3 billion worldwide in 2010 and this is expected to increase to US$6 billion in 2014. Of great concern to the clinical and healthcare communities is the rise in fungal infections, which are resistant to conventional antifungal drugs, as well as increasing reports of resistance development in patients toward antifungal agents. These trends necessitate the urgent development of suitable alternatives to the limited selection of available antifungal agents. Further, most conventional antifungal agents do not completely destroy the fungi but merely inhibit their growth, which may lead to future infections.
A particular challenge facing researchers lies in fungi’s metabolic similarity to mammalian cells. Existing antifungal agents are unable to distinguish between infected and healthy cells, and frequently end up attacking the latter. Hence, patients report hemolysis and nephrotoxicity as treatment side effects.
Leveraging IBM’s polymer synthesis and computational expertise, as well as IBN’s nanomedicine and biomaterials research expertise, the researchers transformed PET, a common plastic material, into novel small molecule compounds that self-assemble in water into nanofibres. Via electrostatic interaction, the nanofibres are able to selectively target fungal cells and penetrate their membrane, killing them in the process.
According to Dr Yi Yan Yang, Group Leader, IBN, “The ability of our molecules to self-assemble into nanofibres is important because unlike discrete molecules, fibres increase the local concentration of cationic charges and compound mass. This facilitates the targeting of the fungal membrane and its subsequent lysis, enabling the fungi to be destroyed at low concentrations. The result is a highly efficient killing strategy that causes minimal damage or toxicity to surrounding healthy cells.”
In vitro studies conducted at IBN demonstrated that the nanofibres eradicated over 99.9% of C. albicans after just one hour of incubation and did not develop any drug resistance, even after 11 treatments. C. albicans causes the third most common fungal blood stream infection in the US. The nanofibres were also used to effectively treat contact lens-associated fungal biofilm eye infection in mice without causing any toxicity to the eye. In comparison, the conventional antifungal drug, Fluconazole, was only able to inhibit additional fungal growth, and the infection exhibited drug resistance after six treatments. Further, Fluconazole was not effective against biofilms.
According to Dr James Hedrick, Advanced Organic Materials Scientist, IBM Research, “As computational predictive methodologies continue to advance, we can begin to establish ground rules for self-assembly to design complex therapeutics to fight infections, as well as the effective encapsulation, transport and delivery of a wide variety of cargos to their targeted disease sites.”
The IBN and IBM scientists have made other recent breakthroughs in antimicrobial research. By combining their antimicrobial polymers with conventional antibiotics or antifungal drugs, they were able to induce the formation of pores in microbial membranes, which promotes the penetration of antibiotics into the microbial cells, and kills highly infectious, drug-resistant P. aeruginosa at significantly lower concentrations when compared to the antimicrobial polymers and antibiotics alone. In addition, the researchers have also fine-tuned their biodegradable antimicrobial polycarbonates to produce polymers with strong and broad-spectrum antimicrobial activity and negligible toxicity to mammals.
IBN and IBM’s research collaboration has resulted in more than 20 platform technologies on drug, protein and gene delivery, as well as macromolecular antimicrobial agents to treat MRSA infections, other infectious diseases and cancers. The research team is now actively seeking pharmaceutical companies to further develop their newest breakthrough for future clinical applications.
(PRA)